Features
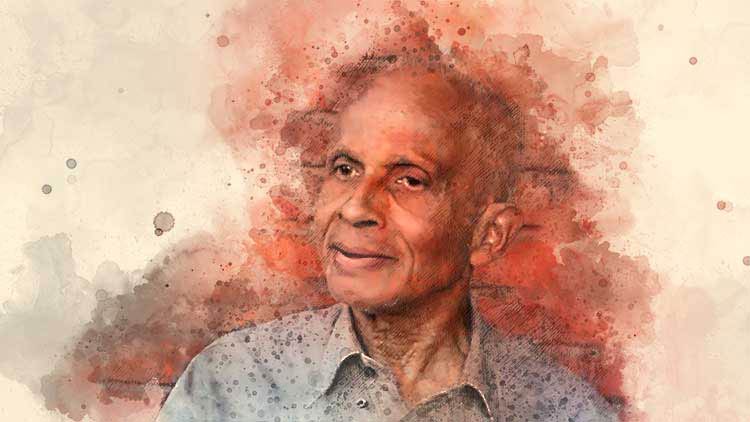
The Life and Times of Dr. Suman Fernando
By Ted Lo
Dr. Suman Fernando, a pioneering thinker in psychiatry, a fearless advocate for social justice in mental health, and the author of several important books on the subject passed away peacefully on January 31, 2025, at his home in London at the age of 93.
Although not widely known in Sri Lanka—the country of his birth, where he lived until the age of 17, and where his extended family continues to reside—Dr. Fernando was a much-respected figure in the field of mental health in the UK.
In 2012, shortly after turning 80, he was interviewed by his longtime friend and colleague, Ted Lo, about his passion for and lifelong dedication to mental health.
Below, we reproduce some of his reflections on the dilemmas of his early life which influenced him to choose mental health as his life’s commitment.
Early Life in Sri Lanka
Suman Fernando: I have always been interested in people’s cultures and backgrounds. Even as a child, I remember reading about African tribes and missionaries like Schweitzer—an interest in the exotic, I suppose. We didn’t use the term ‘multicultural’ then, but my early life was exactly that. Although I came from a Christian Sri Lankan Sinhalese background—my father was a Methodist, my mother an Anglican—our family was not particularly religious. My father often went to sleep in church. He was a doctor but also a politician in a somewhat left-wing party—a sort of armchair left-winger. Our home was frequently visited by people from different religious backgrounds. I remember my mother covering a chair with a white sheet when a Buddhist monk visited, and keeping the dogs away when a Muslim guest arrived, though I never understood why.
I was baptized and later ‘recognized’—a kind of confirmation at around 14 or 15. Methodists formed a small group of a few thousand members, mainly middle class, descended from early colonial-era converts.
For primary school, I attended a girls’ school called Ladies College, which admitted a few boys until the age of 12. It was run by missionaries. My secondary education was at Royal College, the only major state school in Colombo modeled after British public schools, with a principal and some teachers brought in from the UK. Established in 1835—just 20 years after Britain subjugated the country—it soon became a prestigious institution for the emerging middle class. Every morning, we had an assembly with readings from different scriptures—Muslim, Buddhist, Hindu or even secular literature—followed by classroom discussions.
Despite its multicultural setting, education was conducted entirely in English. Speaking Sinhalese or Tamil at school was discouraged; those languages were reserved for communicating with servants. This bred a sense of resentment, one my father often commented on. He criticized the way we were taught to look down on local languages and customs, yet he himself dressed in the manner of what the British called a ‘Westernized Oriental Gentleman’—the origin of the term ‘Wog,’ later used pejoratively in Britain. The British encouraged locals to imitate them, yet simultaneously despised those who did.
Sri Lankan society was deeply class-conscious but multicultural. I had Muslim, Tamil, and Buddhist friends, and there were many Parsi boys at school, some of whom became my closest companions. Lunches were brought from home, and we often shared our food. However, while Colombo’s middle-class life was diverse, the rural areas were different—some villages were homogeneous, while others were mixed. Sri Lanka’s population was composed of Sinhalese, Tamils, Burghers (mixed Dutch or Portuguese descent), Arabs, Chinese, and even an African community—descendants of slaves brought by the Portuguese. The indigenous people, the Veddahs, were few in number.
Studying in England
My father studied medicine in England, as had his father before him. My grandfather trained in Edinburgh in the late 19th century, and my father attended Cambridge and University College Hospital (UCH), just as I did. I left for England at 17 to study medicine. Before securing my place, I had to pass the first MB examination in London, so I attended a ‘cram school’ where foreign students prepared intensively for British university entrance exams.
Finding accommodation was difficult. Many places displayed signs reading ‘No Coloureds, No Irish’—sometimes even ‘No Dogs,’ though dogs faced less discrimination than people. I briefly stayed in a hostel run by Methodist ex-missionaries from China before moving to Cambridge. There, the experience was different—students were well looked after. When I arrived, a porter carried my suitcase to my room.
Students lived in college housing for their first year but had to find private accommodation afterward. In my case, my tutor allowed me to stay in college because he knew I would struggle to find a place elsewhere. However, in my third year, I stayed in a vicarage because the vicar was willing to take in Black students. While there was no overt hostility, an undercurrent of prejudice remained. Cambridge students were polite to each other but condescending toward townspeople. We wore gowns outside college and looked down on non-students. This was the 1950s.
For clinical studies, I moved to London. Though conditions were improving, I disliked the city. Looking back, Cambridge felt like a bubble. Life was different outside the elite universities. At one hospital round, an Australian instructor asked me a question. When I hesitated, he said, “Of course, you people always sit on the fence”—a reference to the non-aligned movement led by India and Indonesia. The other students laughed. I smiled weakly but cried inside.
I often skipped sessions to avoid such treatment, something I later regretted—especially in anaesthetics. Today, medical education has changed; overt racism has diminished, at least in London and major cities. Yet, psychiatry remains resistant to change. The system still fails to adapt to Britain’s multicultural reality and continues to be structurally racist.
Psychiatry and Advocacy
I qualified as a doctor but soon realized I did not enjoy surgery or general medicine. Had I been given a choice, I would have studied English and become a writer. But with a family legacy of doctors, I had followed expectations. Psychiatry intrigued me, so I pursued it despite the challenges. I returned to Sri Lanka in 1960 for work experience at the Angoda Mental Hospital near Colombo, which was recognized for psychiatric training. The conditions were appalling, but I learned a great deal. A Viennese neuropsychiatrist, who spoke neither Sinhalese nor Tamil, would sit beside his patients, place an arm around them, and speak softly unlike local psychiatrists, his patients improved. That moment reshaped my view on ethnic matching—it is not always necessary.
Back in England, I became more vocal about psychiatric practices, particularly their injustices toward racial minorities. I opposed over-reliance on medication and compulsory hospitalization. I resisted the use of electroconvulsive therapy (ECT), except in life-threatening cases. Later, I stopped using it altogether.
My advocacy work intensified in the 1980s. I hoped for systemic reform, but psychiatry remains entrenched in outdated models, perpetuating racial disparities. One of my most recent projects has been challenging the schizophrenia diagnosis, advocating for a less rigid, more inclusive approach.
Even now, I remain engaged in improving mental health care in Sri Lanka, working alongside British and Canadian colleagues. Reflecting on both countries, I see Britain becoming more tolerant while Sri Lanka, at times, seems to regress.
At 80, I remain tireless in my advocacy. I hope this conversation helps others understand the complexities of mental health and cultural identity. As the evening darkened, we ended our discussion, though Suman Fernando showed no signs of fatigue. It was a privilege to speak with him, and I hope this record allows others to share in this remarkable journey.